Controlling Blood Supply Chain
Controlling Blood Supply Chain
The blood supply chain is a complicated, and costly process. However every step of it is completely necessary to save lives around the world. Within the blood supply chain there are numerous challenges, not least of which is regulating the environment in which blood supply products are maintained.
Temperature control is a necessary practice at every step within the blood supply chain. If even one step fails to maintain proper temperatures, the blood supplies may spoil or degrade.
How the Blood Supply Chain Works
Blood supplies are sent to their final destination through the cold chain. The cold chain is essentially a temperature controlled transportation process. However, the cold chain involves every aspect of shipping an item, from packaging it, to loading it, transporting, unloading it, and ultimately storing and receiving it at the end facility. That also includes all materials, vehicles, equipment, and personnel that take part in the shipping.
Outside of the cold chain, blood supplies need to go through their own chain of procedures, including:
Donor collection
This is the first step in the blood supply chain. The donor goes to a center or donation site and gives their blood.

Initial storage and transport
Once the donor gives blood, the donation site personnel properly store the supply. After storing, the blood has to go to a blood bank. Depending on the distance to the blood bank, the supplies may need refrigeration. Blood can remain at ambient temperatures (68-75 degrees fahrenheit), for up to six hours before processing. However, transportation to a blood bank can often take longer, so most blood supplies go into cold storage containers to preserve them.
Arrival at the blood bank
Once the blood arrives at the blood bank, the personnel test it, process it, and properly store it. Blood may undergo processing to extract specific components (such as platelets or plasma) for special transfusions or treatments. Depending on whether it’s processed into certain components, it has different storage requirements.
Order for transport
Once a medical facility needs supplies from the blood bank, they order them, and the blood supplies are packaged for transport. Again, the blood supplies go into cold storage, with temperatures specific to their storage needs. This is where blood again enters the cold chain, and goes to the medical facility in need. Blood supplies should ship in climate regulated transport, like a refrigerated truck.
Arrival at the destination
After the transport, blood supplies arrive at their destination. According to regulations, staff should test the blood supplies to ensure a proper temperature. Again, the blood supplies go into temperature controlled storage that meets their specific requirements.
Distribution to the patient
After going into storage at the hospital, the blood supplies stay in strictly regulated temperatures until they’re needed. Once a patient needs the blood supplies, they’re prepared and delivered to the patient for treatments and transfusions.
Opportunities for Error
The blood supply chain includes many steps, and each step presents a plethora of opportunities for error. Each error in turn is another chance that these valuable supplies might be wasted. Blood supplies do expire, and issues with temperature management, unforeseen delays, and more may decrease the supply’s viability.
Common opportunities for error include:
- Transportation delays
- Failure to follow proper protocols
- Cold shipping equipment failure
- Miscommunications
- Unnoticed temperature excursions
- Errors during collection
- Improper packaging
- Packaging that lacks proper insulation
What Waste Costs in the Blood Supply Chain
Blood might be donated, but the blood supply chain is far from cheap. Blood has to undergo testing, processing, storage, and transportation in very strict environments, which cost both patients and providers. Within Europe and the United States, blood product transfusions cost, on average, between $522 and $1,183 (Shander et al. 2010; Abraham and Sun 2012).
According to a study published in 2014, blood waste in surveyed hospitals can range from 1.93% to 30.7%, and averages 9.8%. In the United States, blood supply and component waste typically ranges from 1% to 5%, according to the American Journal of Clinical Pathology.
That means that anywhere up to one million units can be wasted. Ultimately, this can cost between $46 million to $230 million each year. Unfortunately, these wastes aren’t primarily due to blood products reaching their expiration dates.
In fact, much of this blood product waste is ‘in-date.’ That means that these products are unusable due to factors outside of a typical expiration date. Some of the causes are improper procedure, failure to return unused products, and improper storage, especially when the blood reaches unacceptable temperatures.
Reducing Waste in the Blood Supply Chain
In the United States alone, wastage of blood supplies can cost hundreds of millions of dollars annually. As mentioned above, much of this waste isn’t due to normal expiration, and is therefore preventable. However, the blood supply chain is highly complex, and involves many steps and moving parts. Therefore, the solution to reducing blood product waste has to simplify the process and allow greater control of the blood supply products.
Blood products go through the cold chain to reach their final destination. Within the cold chain are multiple opportunities for blood supply spoilage, even when they’re undetected. Ultimately, a more accurate, thorough method for monitoring blood products in transport is one key to preserving the supply.
An advanced temperature sensor can record temperatures in the cold storage from the beginning of transport to the end destination. These temperature sensors go inside the insulated storage along with the blood products. Then, the sensors log temperature readings every few minutes. This continues as long as the supply is in transit. If, for any reason, the supplies have a temperature excursion, it will be reported upon reaching the final destination.
This solves the issue of blood products losing integrity due to unnoticed temperature excursions. Once the blood supplies arrive, personnel unpack the sensor with the supplies, and upload the information from the sensor. A historical log showing every reading is available in mere moments, verifying the validity of the products.
Another issue causing unnecessary waste happens on-site. Whether in a blood bank, hospital, or other biorepository, medical freezers and refrigerators can malfunction. CDC regulations state that temperature readings should be taken at least twice daily. However, like an unnoticed temperature excursion during the cold chain, this may mean missing a temperature variation.
Much like sensors can monitor blood supply during shipping, a temperature logger can monitor supplies on site. The temperature logger simply goes into the cold storage, near the sensitive supplies. Then, much like the sensor, it takes readings of the temperature every few minutes. It uploads temperature readings via a gateway, and transmits the data to a system that shows readings over time.
Related:
Regulating Blood Temperature – Blood Banks and Biorepositories
Blood is an expensive business, even if the base product comes from donations. That’s why regulating blood temperature for blood banks and biorepositories is more important than ever. Worldwide, current blood supplies sit at around 100 million units. Each unit (which includes about 450 milliliters), requires extensive supervision, regulation, transportation, processing, and temperature control.
Best Practices for Storing Blood
Blood banks and biorepositories have to adhere to certain regulations and practices to ensure viability. Many of the best practices for storing blood relate to temperature, which can be difficult for staff to manage. Because temperature regulation relies heavily on equipment, staff may struggle to record and maintain proper temperatures.
The common best practices for storing blood include:

Practicing Proper Storage Length
In general, most blood specimens are used within six weeks of storing them. However, over time, red blood cells begin losing the ability to carry oxygen. New research is showing new data that may cause us to rethink this timeline, though. Johns Hopkins University released a study in 2013 showing that blood may start losing the ability to carry oxygen by three weeks. This is because red blood cells lose membrane flexibility over time, which is what allows them to carry oxygen.
Storing at Correct Temperatures
Various blood components need different storage temperatures to remain stable. For example, whole blood can be stored between 2 and 6 degrees celsius. On the other hand, components like plasma (also called fresh frozen plasma, or FFP) need to be frozen at temperatures between -20 to -27 degrees celsius.
The equipment storing the specimens, such as blood refrigerators and freezers, cannot be the typical residential type. They must be certified to specific standards, and have the ability to maintain low enough temperatures.
Verifying Temperatures
Current CDC guidelines dictate that storage temperatures need verification twice daily. Once at the beginning of the day, and again at the end of the day. Likewise, the temperature should be checked whenever retrieving specimens from the cold storage. Staff must record the temperature readings from the beginning and end of the day. These records should be kept for several years, although the timeline does vary by region and regulatory agency.
Maintaining Proper Records
Keeping proper records is crucial with any human biospecimen storage. While the CDC recommends recording temperatures twice daily, other organizations have even more stringent rules.
For example, the MEDIC organization dictates:
- Storage units must record temperatures every four hours
- Any equipment failure must be recorded and reported
- Alarms for temperature excursions should be reported and properly documented
- If a blood refrigerator fails, temperatures should be recorded every 30 minutes until repaired
- Supervisors must inspect all samples in storage daily, and record their review
- Recorders and thermometers must read within 1 celsius of another
- If recorders and thermometers show a greater difference, they must be calibrated
Depending on the regulatory agency, there are various levels of recording for specimens. This can place extra burden on the staff, although it’s necessary to verify the viability of blood samples. If biorepositories or blood banks use automated loggers, much of this extra work is avoidable. Not only that, but staff can ensure more accurate records with minimal effort.
Simplifying the Process
The aforementioned ‘best practices’ center primarily on regulation. That’s nothing to say of the other practices blood banks and biorepositories must adhere to, regarding sampling, testing, and distributing. Every step of the blood chain is a complex machine of its own with numerous moving gears.
With such a delicate and complex process, there are endless opportunities for error. Not only that, it also takes a lot of labor to manage. Using the proper equipment to aid regulating blood storage is the first step to simplifying the entire process. While some blood storage refrigerators do contain recording units, few record temperatures more frequently than every few hours. Should an alarm system also fail, an entire storage unit of blood specimens can spoil.
A temperature logger essentially eliminates all these issues, in one simple step. Staff can install the temperature logger in the storage unit and let it do the work of recording and setting alarms for temperature failure. These loggers also do the work of recording all temperature readings, as well as alarms. Then, all the logs are stored for future reference.
Temperature loggers record temperature readings every few minutes, far beyond what any regulatory agency requires. Should a refrigerator alarm fail, the temperature logger sends an alert to designated staff and supervisors. These loggers are even a failsafe in case of a power outage. While a storage refrigerator can’t send an alarm during a power outage, the logger will. Because readings are uploaded every few minutes, the system detects a critical failure when the readings are absent, and sends out an alert.
Related:
Blood Sample Transport and Storage
Blood samples require specific temperature regulation as they undergo both processing and storage. A large part of their usefulness depends on proper procedures. One of the largest issues occurs during transportation, and entire shipments of specimens can be destroyed without proper handling. With blood (and blood components) more in demand than ever, it’s crucial that these specimens go through the cold chain and reach their final destination without losing integrity.
| Condition | Acceptable Temperatures | Viability Time |
| Pre-processing | 20-24C (68-75F) | 6 hours or less |
| Storage (pre and post processing) | 2-6C (35-43F) | 35 days (estimated) |
| Processed, transporting | 2-10C (35-50F) | 24 hours or less |
The guidelines for transporting blood components vary based on the component in question (plasma, red cells, white cells, platelets). However, these are generally accepted storage conditions within the viability time (or time in storage), endorsed by the NBTC (National Blood Transfusion Council).
Blood in the Cold Chain
Proper handling of human biospecimens, and in particular blood, is crucial to preserving their integrity. It’s not even the ultimate condition the repository receives them in that determines their viability. Many blood samples and stocks go through cold chain transport to reach their final destination. Essentially, the cold chain is a term used to describe the process of shipping products that require freezing or refrigeration through both their transport and storage at the destination.
Cold chain transport can include refrigerated trucks, containers within planes (air transport), cold cars in trains, and even shipping by sea (boats and freighters). No matter the method, the important aspect is that the goods remain cold, and at acceptable temperatures to preserve their integrity.
The blood and medical cold chain involves everything from storage and transport, to the equipment and workers involved.
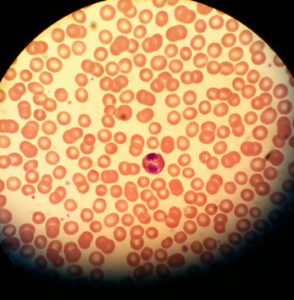
The Components of Blood
There are various different components of blood that go through the cold chain to reach their final destination. Most people are familiar with whole blood, which is essentially blood drawn from the veins. However, there are other components of blood that are just as essential to the medical industry.
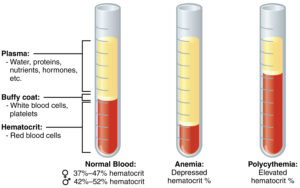
The most crucial components of blood include:
Whole blood – Blood taken in whole form, without any separation
White blood cells – Also known as granulocytes. These are components of blood that help the body fight off infections. These are much less common, because of their short term use and the possibility of ill side effects.
Red blood cells – Often abbreviated as RBC. These are the blood cells that help the body transport oxygen. Red blood cell transfusions are far more common, especially in patients with a low blood count.
Plasma – This is part of the blood, and when separated from other components, it has a somewhat transparent, yellow color. Plasma supports blood cells, although plasma transfusions are more common for people with poor blood clotting.
Platelets – These help with blood clotting, and while they are fairly common for transfusions, they have a short viability time. Platelets often last for only between 8 and 10 days.
For more information about the components of blood, and types of transfusions, see the AAMDS Foundation website.
Keep in mind that no matter what type of component goes through shipping, a constant temperature is crucial. Fluctuating temperatures can have serious consequences on the quality and viability of any blood component.
The Neo Sensor measures all temperature ranges for storing blood components and beyond (-40℃ to 70℃).

How to Transport Blood in the Cold Chain
Transporting blood, like any medical product, is no simple process. From the collection site to the packaging, all the way to the final destination, every step is important. Transporting whole blood is one thing, while transporting the different components of blood is another thing entirely.
These are guidelines for how to properly transport each blood component, and the temperatures they need to stay at:
Whole blood
Whole blood is perhaps the easiest to ship, because it doesn’t require extensive refrigeration. However, it does need a quick transport process. Before processing whole blood it can undergo transportation at between 68 and 75 degrees fahrenheit (20-24 celsius). This temperature range is safe, but only for up to six hours.
After six hours, whole blood must be stored at much cooler temperatures. For extended storage and transportation, whole blood should stay between 35 and 43 degrees fahrenheit (2-6 celsius). This rule applies whether the whole blood is in the pre or post processing stage. Once between 35-43 degrees, whole blood is viable for approximately 35 days.
White blood cells
While white blood cells aren’t as common as other types of blood transfusion, they still require strict shipping and storage temperatures. Once white blood cells undergo processing (and are considered stable), they have even greater temperature tolerance than whole blood, for a limited period of time. WBCs (white blood cells) can stay at temperatures up to 86 degrees fahrenheit (30 celsius) for up to five days.
After the five day mark, white blood cells need more extensive temperature control. They should then be in a freezer, or temperature controlled shipping unit, at -4 degrees fahrenheit (-20 celsius).
Red blood cells
The way we store red blood cells (RBCs) is undergoing a change from the past regulations. In previous decades, a temperature range of 33.8 to 42.8 degrees fahrenheit (or 1 to 6 celsius), was acceptable for long term storage. While that is still common practice in many medical fields, many organizations are beginning to change their recommendations for RBC storage.
Now, many organizations recommend storing red blood cells between 35.6 and 39.2 degrees fahrenheit (2 to 4 celsius). Storing them at extremely low temperatures (and freezing them) essentially destroys the cells. Higher temperatures greatly decrease their ‘shelf life.’ Keeping RBCs within the proper temperature range not only slows potential microbial growth, but also limits the cell metabolism (glycolysis).
Plasma
Plasma has very strict storage and transport temperature requirements. This is one of the reasons plasma is frozen once separated from the whole blood. While plasma can stay in ambient temperatures for up to 24 hours, most medical organizations recommend no more than 6 hours without freezing.
Once frozen, plasma should be kept between -4 and -16.6 degrees fahrenheit (-20 to -27 celsius). However, before that, plasma needs to undergo a fast freezing process that brings it below -22 degrees fahrenheit (-30 celsius) to preserve it.

While in transport, the plasma must stay cold, although a temperature excursion up to 5 degrees fahrenheit (-15 celsius), is acceptable. However, this is only if the temperature excursion lasts less than 72 hours (consecutively), and does not occur more than once during transport.
Platelets
Platelets have different temperature requirements depending on whether they’re in transport or storage. Not only that, platelet temperature storage also depends on whether continuous and gentle agitation is possible.
While in transport, platelets are safely within temperature requirements when they’re between 33.8 and 50 degrees fahrenheit (or 1 to 10 celsius). However, once they arrive, they need to be stored between 33.8 and 42.8 degrees fahrenheit (1-6 celsius). This is assuming the constant agitation isn’t feasible.
When continuous agitation is possible, platelets are in a safe temperature range between 68 and 75 degrees fahrenheit (20 to 24 celsius). However, because a safe, constant method of agitation isn’t always possible or cost effective, many companies choose to cool platelets instead.
Blood Quality Problems From the Cold Chain
There are many issues concerning blood quality when samples go through the cold chain. Of course, the cold chain is the major method of making sure blood arrives at the repositories, labs, hospitals, and other centers that need it.
Standard regulations require reading the temperature both before shipping and after arrival. Unfortunately, this does not ensure a high quality specimen. Refrigerated shipping containers can bring temperatures low enough to ensure a proper reading upon arrival. However, the specimens might still undergo a temperature excursion that goes undetected.
For instance, if a truck’s shipping container is opened during the trip, the specimens can reach unacceptable temperatures. However, if the container is closed back up, and has time to cool back down to proper temperatures, the recipient might never know the specimens were compromised.
Even if blood specimens arrive at the proper temperature, a temperature excursion affects their quality, and their viability.
The biggest risks when blood goes through the cold chain include:
De-oxygenation
This is a large risk, in particular for whole blood and red blood cells. Red blood cells carry oxygen from the lungs to the rest of the body. Once these specimens are collected, they’re only viable (without refrigeration) for a short time. After that time, they begin losing their ability to carry oxygen. A temperature excursion, whether during shipping or storage, can ultimately negate one of the biggest reasons for using it for a transfusion.
Expiration
Any time blood specimens fall outside of proper temperatures shortens their time before expiration. The longer blood components are in temperature excursions, the less time they can be used for. In certain instances, like with plasma, blood components can tolerate temperature excursions for a limited time. However, that is only if the specimens still stay within a certain temperature range (i.e. plasma can be at -15 celsius, rather than the advised minimum of -20C, but only for up to 72 hours, and it can only happen once).
Microbial growth
With any temperature sensitive product, bacteria and other microbes can develop in the right conditions. Even refrigerated products are at risk for some microbial growth. While refrigeration won’t kill microbes, it will delay or halt their growth. Freezing may kill some germs and bacteria, although in most cases it doesn’t. In fact, it typically puts them into a sort of stasis which actually preserves them.
iMatrix Products for Blood Supply Chain: